Gut Feeling: How Healing Your Microbiome Could Help Fight Cancer
Restoring gut health may enhance cancer treatment and reduce side effects
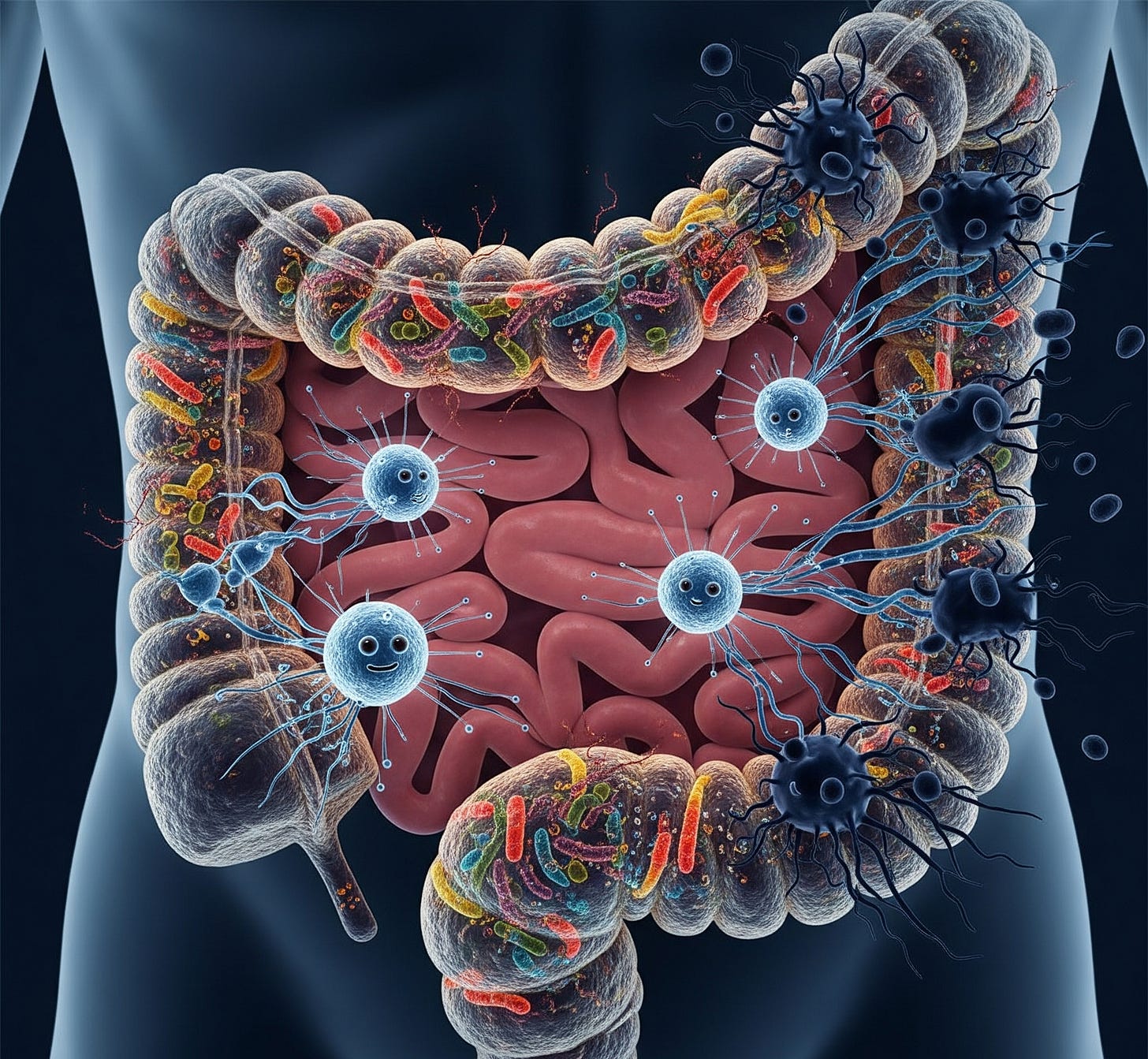
What if the key to treating cancer more effectively lies not just in chemotherapy or immunotherapy—but in your gut? It may sound surprising, but growing research shows that the gut microbiome—the community of trillions of bacteria living in our intestines—plays a critical role in how well cancer therapies work and how well our bodies tolerate them.
From boosting the immune system to modulating inflammation and drug metabolism, restoring gut balance is emerging as a powerful companion strategy in the fight against cancer. As researchers uncover this complex relationship, innovative treatments like microbiota transplants, prebiotic diets, and targeted probiotics are moving from the lab to the clinic.
The Gut-Cancer Connection: More Than Digestion
Our gut isn’t just for digesting food—it’s also home to over 70% of the immune system. This means the microbiome influences not just digestive health, but also immune responses, inflammation, and even cancer progression.
When the gut microbiome is out of balance—a condition called dysbiosis—bad bacteria can thrive while beneficial bacteria dwindle. This imbalance has been linked to:
Increased systemic inflammation
Weakened immune surveillance
Poor response to cancer immunotherapy
Greater toxicity from chemotherapy
In contrast, a diverse and healthy microbiome appears to enhance the efficacy of treatments like immune checkpoint inhibitors and may even help prevent certain cancers from developing in the first place.
Immunotherapy and the Microbiome: A Surprising Partnership
Immunotherapy, which stimulates the body’s immune system to attack cancer, has revolutionized treatment for melanoma, lung cancer, and some blood cancers. But it only works in 30–50% of patients. Why? One reason may lie in the gut.
A groundbreaking 2018 study published in Science showed that melanoma patients with diverse gut microbiota responded much better to anti-PD-1 immunotherapy than those with poor microbial diversity. Patients with beneficial bacteria such as Akkermansia muciniphila and Bifidobacterium longum had stronger immune responses and longer survival.
Further research confirmed that fecal microbiota transplantation (FMT)—transferring stool from a cancer patient who responded well to immunotherapy into a non-responder—could reprogram the gut and restore treatment sensitivity.
Latest Advances: What 2024–2025 Research Reveals
1. Clinical Trials Using Fecal Transplants
Several clinical trials are underway testing FMT in combination with cancer therapy. A 2024 study in Nature Medicine showed that advanced melanoma patients who received FMT from successful immunotherapy responders had a 40% improvement in progression-free survival.
Researchers at MD Anderson Cancer Center and Memorial Sloan Kettering are also exploring personalized microbiota modulation—using a patient's own bacteria, cultured and rebalanced, to improve outcomes.
2. Targeted Probiotics for Cancer Support
New-generation probiotics, engineered to deliver anti-cancer molecules or stimulate specific immune pathways, are entering early trials. For example, Lactobacillus rhamnosus has shown promise in reducing gut inflammation during chemotherapy in colon cancer models.
Companies like Vedanta Biosciences and Synlogic are developing live biotherapeutic products (LBPs)—drug-like probiotics aimed at enhancing the gut's immune training capacity.
3. Prebiotics and Cancer Prevention
Prebiotics (fiber-rich foods that nourish good bacteria) may reduce cancer risk. A 2025 meta-analysis found that high-fiber diets were linked to a 20% lower risk of colorectal cancer, especially when they promoted short-chain fatty acid production (like butyrate), which protects against DNA damage and tumor formation.
Chemotherapy Side Effects and Gut Restoration
Chemotherapy is notorious for its side effects—nausea, diarrhea, fatigue. These are often not caused by the drugs themselves, but by the damage they do to the gut lining and its microbiota. Research now shows that restoring the microbiome can:
Reduce inflammation
Speed up gut barrier healing
Alleviate fatigue and brain fog
Support appetite and nutrient absorption
In 2025, researchers at Stanford demonstrated that a synbiotic regimen (a combination of probiotics and prebiotics) given during chemo reduced gastrointestinal side effects by 35% and lowered inflammation markers like IL‑6 and TNF‑α.
Cancer Types Where Gut Health Matters Most
While gut restoration can benefit most cancers, it’s especially impactful in:
Colorectal cancer – where the microbiome directly influences tumor growth
Melanoma – where gut microbes modulate immunotherapy response
Lung cancer – where dysbiosis may impair immune checkpoint inhibitor efficacy
Leukemia/lymphoma – where gut health affects chemotherapy tolerance
From Stool Pills to Designer Microbiomes
Today’s gut-restoring strategies go beyond yogurt and fiber. Some cutting-edge approaches include:
Oral microbiome capsules (e.g., SER-155)
Autologous FMT – using the patient’s own stool banked prior to chemotherapy
Microbiome-modulating diets, tailored to enhance immunotherapy
Smart probiotics engineered to sense tumor environments and deliver drugs
What Patients and Caregivers Can Do
If you or a loved one is undergoing cancer treatment, consider the following gut-friendly tips:
· Ask your oncologist about microbiome testing or supportive care trials
· Eat a diet rich in prebiotics: oats, garlic, onions, flaxseed, legumes
· Limit unnecessary antibiotics, which disrupt microbiota
· Discuss safe use of probiotics tailored to your treatment
Conclusion
The gut microbiome is no longer just a digestive player—it’s a powerful ally in the fight against cancer. From influencing immune responses to reducing chemotherapy side effects, restoring gut health offers a new frontier in oncology. With targeted therapies, designer probiotics, and fecal transplants moving into mainstream care, we’re witnessing a shift where the phrase “trust your gut” takes on a whole new meaning.
In the years ahead, cancer treatment may no longer begin in the infusion room—but in the gut.
Medical Disclaimer:
This article is for informational purposes only and is not a substitute for professional medical advice. Always consult your doctor before making any medical decisions or starting new treatments.